—Injuries, functional disorders and the study of other causes of illness were at the centre of the medical revolution of the nineteenth century.—
Disease has always been present in human life. The way in which it has been understood, however, has changed substantially over time: what produces it, why it does this, how it manifests itself, how one can find out that someone is suffering from it and how it is possible to prevent and treat it. From the sixth century AD on it has been possible to identify, with some certainty, the diseases described in various historical sources. Only fragmented information on infectious diseases is available prior to this time. In the tropical rainforest, the warm and humid climate led to contact with microorganisms such as the malaria Plasmodium. When the habitat became the Savannah, a warm but dry climate opened the door to new parasites such as Trypanosoma, the cause of sleeping sickness, which would then spread. In the Neolithic, the new activities developed by humanity, such as agriculture and livestock, put us in contact with germs that lived in the water, such as the hookworm, which penetrated through the sole of the foot, when rice began to be cultivated. There was also the passage of parasites from animals to humans, particularly when increased contact with domestication and livestock occurred. This was the case with the tuberculosis bacillus, which initially infected animals such as pigs, and became a cause of human disease when this animal was domesticated. Other diseases were brought about by technological changes. For example, the discovery of fire allowed foods to be cooked, which led to an increase in carbohydrate consumption and the presence of tooth decay.
Throughout history there have been different interpretations of the event of getting sick, these being based on empiricism, beliefs or science. Disease can be approached from empiricism, when one accepts what is repeated without the need to give a rational explanation; from beliefs, if this is based on the existence of supernatural forces (magical beliefs) or of superior beings (religious beliefs) that act on man and are responsible for his illnesses; or from science, when any approach to disease is based on logic and reason. Our current scientific medicine comes from classical Greek medicine, based on the so-called humoral theory according to which there were four humours or fluids in the human organism: blood, yellow bile, black bile and phlegm. When these humours were balanced, that is, in the right amounts, their composition -the result of the mixture of the four elements (air, water, fire and earth) in certain proportions- was correct and they could flow unhindered through the organism. Therefore, the individual was healthy, free of disease. When any of these parameters became unbalanced, the morbid entity appeared. This way of interpreting human pathology would stay the same, with few changes, until the mid-nineteenth century, when there was a genuine clinical revolution.
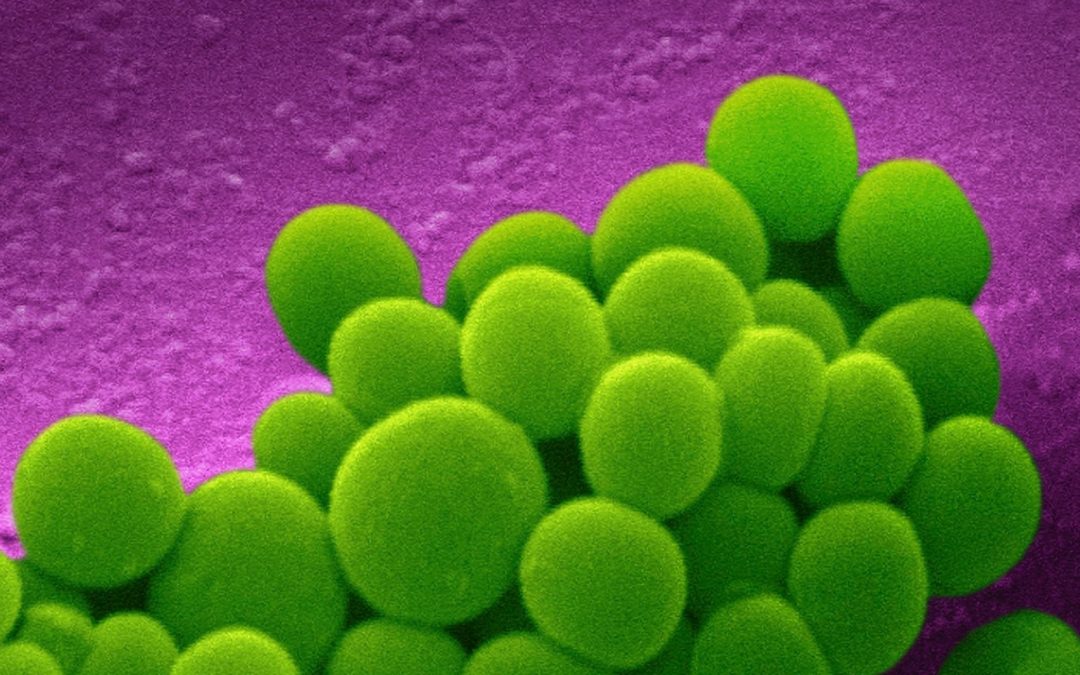
Staphylococcus aureus bacteria. Wellcome Collection.
The theory of humours proved insufficient to explain the causes and manifestations of disease, while the consolidation of disciplines such as physics and chemistry provided new diagnostic and therapeutic procedures. The development of anatomy from the sixteenth century on had made it possible to identify the structure of the healthy body through the frequent use of the dissection of corpses from the late Middle Ages in the medical faculties of European universities. In the first third of the nineteenth century when morphological alteration or injury began to be related to specific diseases to become the central focus of the disease: its cause, that which was responsible for the signs and symptoms that the patient presents, the test to establish a diagnosis and what the doctor will have to eliminate to obtain the cure. The development of a specific scientific discipline for its study, pathological anatomy, made it possible to explore not only macroscopic but also microscopic lesions, with the help of improvements made to optical instruments such as the microscope. In other things, thanks to these improvements, it was possible to interpret the organic lesion as the sum of the altered cells in the affected area, as Rudolph Virchow affirmed in 1858 in his work Cellular pathology. The exploratory techniques developed for this purpose sought, as in present-day medicine, to locate the lesion in the patient’s body by means of the marks or signs it produced, without having to wait for the autopsy. Among these are those that manage to locate it by touch, such as palpation; those that collect the changes in sound produced in the area where the lesion is found, such as percussion and auscultation; or those that manage to visualise it through various resources, for example, endoscopies or diagnostic imaging techniques, such as radioscopy and more recently, computed axial tomography or magnetic resonance imaging.

Stethoscope (London, 1891, National Library of Medicine). U.S. National Library of Medicine.
For those diseases in which this structural explanation was insufficient, they were addressed through the study of alterations in organic functions (or dysfunctions), sometimes through measurements based on physical and chemical analysis. In this way, solutions were provided for the understanding of diseases such as diabetes in the central decades of the nineteenth century. A urine analysis, for example, made it possible to detect the presence of glucose or its increase in the blood of patients with pancreatic dysfunction. On the other hand, the application of the thermometer allowed increases in body temperature to be detected, a physiological variable whose regulation is part of the basic functions of the organism. Another example is the cardiogram that allows us to visualise the alterations of the electrical activity in the heart, responsible for its functioning, in a similar way that the electroencephalogram does with the electrical activity of the brain.
Despite all these achievements, an important group of morbid alterations fell outside this explanatory framework and their cause as a guiding thread of all their manifestations and therapeutic possibilities was sought. Pathogenic causes external to the organism of physical origin (water, cold, heat, electricity), chemical (toxic or poison) and biological (parasites, bacteria) were analysed, as well as internal causes, such as the biological make up and genetic inheritance of the individual. This causal or etio-pathological approach proved particularly fertile in the field of infectious diseases: the discovery of microorganisms as causative agents allowed diagnosis, prevention and treatment to be approached from the last quarter of the nineteenth century on.
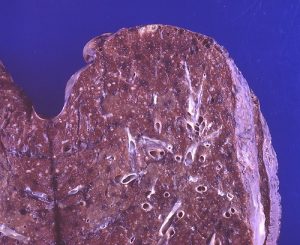
Lung lesion due to miliary tuberculosis. Flickr.
In this way, the laboratory became an indispensable setting for clinical diagnosis, as it was the place where the analysis of organic fluids or pathological samples was carried out. It also played a crucial role in treating diseases as an area for making medicines. A specialised laboratory, the bacteriological laboratory, became an essential part in the diagnosis, prevention and treatment of infectious diseases, with the development of techniques for the growing of microorganisms, detection of antibodies and the manufacture of serums, vaccines and antibiotics.
Handwashing, a routine action before exploring a patient, marked the beginning of disinfection techniques in two fields of medicine. In obstetrics, the contribution of the Hungarian doctor Ignaz Semmelweis in the prevention of postpartum infection through the use of handwashing with disinfectants before exploring the women in labour was essential. In surgery, Joseph Lister, after reading Louis Pasteur’s first works on yeasts as the microorganisms responsible for fermentations, considered that these microscopic living beings were the causes of hospital gangrene, a very serious infection that appeared with high frequency after trauma or surgery and began to use disinfectants to remove them from the operating rooms and surgical material.

Samples in a laboratory (Adrian Wressell). Wellcome Collection.
Pharmacological treatment of infectious diseases was aimed at finding medicines that would eliminate the specific microorganism that caused them. The German doctor Paul Ehrlich coined the term ‘magic bullet’ to refer to the substance intended to impact and destroy the microbe. He thus designed Salvarsan, an arsenic compound that apparently eliminated Treponema pallidum, the etiological agent of syphilis. The subsequent development of antibiotics had the same objective, the elimination of the microorganism responsible for infection. The change in the causal paradigm of infectious diseases was particularly significant, leading to the constitution of medical microbiology as a scientific discipline and allowing progress in control and eradication. The journey through the following sections allows us to learn about the change in the explanation of diseases and the understanding of their etiology, diagnosis, prevention and treatment, a true clinical revolution developed over the nineteenth century and the first decades of the twentieth century.
Mª José Báguena Cervellera
IILP-UV
How to cite this paper:
Báguena Cervellera, Mª José. Clinical revolution. Sabers en acció, 2021-01-13. https://sabersenaccio.iec.cat/en/clinical-revolution/.
Find out more
You can find further information with the bibliography and available resources.
Recommended reading
Duffin, Jacalyn. History of Medicine: A Scandalously Short Introduction. Toronto: University of Toronto Press; 2010.
Jackson, Mark. The Oxford Handbook of the History of Medicine. Oxford: Oxford University Press; 2011.
Studies
Laín Entralgo, Pedro. Clásicos de la medicina: Laënnec. Madrid: CSIC; 1954.
Sources
Bernard, Claude. Edición a cargo de José Luis Barona. Barcelona: Península; 1989.
Cajal. Antología. Edición a cargo de José María López Piñero. Barcelona: Península; 1986.