—How we learned to take aim in a chemical sense in the history of medicine.—
The discovery that specific microorganisms were responsible for infectious diseases led to the search for therapeutic substances to eliminate them. Serotherapy was used, by administering selective antibodies present in the serum that neutralise the action of the infectious agent responsible for disease. The German physician Paul Ehrlich (1854-1915) called them ‘magic bullets’ because they target the pathogenic organism without damaging the cells of the body. Ehrlich applied previous studies on the use of dyes in the staining of human tissues in his research on specific serums. These dyes were specific chemical reactions between dyes and tissues and, in turn, could be used as dyes for bacteria. While working on techniques for staining the tuberculosis bacillus in 1888, he contracted this disease. After two years of travelling through Egypt in search of a dry climate that could cure him, he returned to Berlin and became interested in immunology. From the study of two plant toxins, ricin and abrin, in 1981, he found that, if ingested, the organism produced antitoxins or antibodies, coining the latter term himself, demonstrating that the immunity they gave rise to was specific and that serum antibodies destroyed the toxins. His immunological research led him to the measurement of immunity, which resulted in the law of constant proportions: a certain amount of antitoxin neutralises a certain amount of toxin, as well as the differentiation between active and passive immunity. The latter is acquired by the newborn in the mother’s womb and through milk, this being of short duration.
Alexander Fleming (1881-1955). Wellcome Collection.
In the same year of 1891, Ehrlich began working at the then recently inaugurated Institute of Infectious Diseases, run by Robert Koch. There he developed a method to achieve adequate production of anti-diphtheria serum in horses by repeated toxin injections. Given the very different results obtained in Europe with the application of anti-diphtheria serum, which made it difficult to compare its effectiveness, Ehrlich prepared a standardised serum, a standard antitoxin against which he tested the toxins used in Europe. In 1896 he was appointed director of the Royal Institute for Serum Research and Evaluation, which three years later moved to Frankfurt as the Royal Institute for Experimental Therapy, where he continued his research on anti-diphtheria serum and developed his immunological side-chain theory. According to this theory, the cells have receptors or side chains on their surface that specifically bind to the different toxins that penetrate the organism by means of a key-lock coupling. The cell reacts by producing more side chains, which are released into the blood where they can bind to new specific antigens and block them.

Annotations by Paul Ehrlich with the chemical formula of Salvarsan. Wellcome Collection.
However, there were a number of infections in which serotherapy was ineffective. In these cases, Ehrlich proposed using chemicals and replacing serotherapy with chemotherapy. The main challenge was to find therapeutic agents that had a high affinity for the germ and a great lethal potency, but at the same time did not damage the cells of the host organism. In his words, ‘we must learn to aim and aim in a chemical sense.’ So ‘magic bullets’ were needed, which were chemicals that attacked the parasites and only the parasites. To achieve this, therapeutic substances had to be synthesised by chemical means and tested on experimental animals until the appropriate chemotherapy was found. In 1891, he carried out his first work on antimicrobial chemotherapy. Using again a dye, methylene blue, it was found that its administration to patients with malaria killed the plasmodesmata responsible for the disease, having a specific appetite for these parasites and not being toxic to the body. Back in Frankfurt, he resumed his research on anti-infection chemotherapy, especially from 1906 when he also began to direct the Georg-Speyer Institute for Chemotherapy Research, created for him by a private foundation. He focused on the case of syphilis, produced by a Treponema, Treponema pallidum, discovered the year before. Ehrlich tested different arsenic derivatives until he found the appropriate one in 1910, having tested 606. He called it ‘Salvarsan’, the ‘arsenic that saves’. Before it was marketed, he distributed 65,000 samples around the world to test its effectiveness. Due to the side effects it produced, two years later and after 914 trials, he developed a new drug that was more soluble and easier to use: ‘Neosalvarsan’.
Gerhard Domagk (1895-1964). Wellcome Collection.
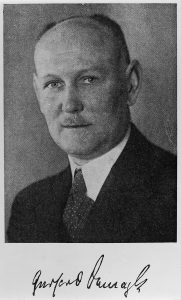
The next effective group of chemotherapeutic agents were sulfonamides, which resulted in a significant decrease in morbidity and mortality caused by streptococci. In 1932, the German bacteriologist Gerhard Domagk (1895-1964) tested Prontosil, a red dye of the sulfonamide group, which was effective against streptococci in mice but he had doubts about its effect on humans. Three years later, when his daughter contracted an infection with these germs after being pricked by a needle and was about to have her arm amputated, he applied Prontosil and the infection disappeared. Domagk concealed this success so as not to influence the clinical trials being conducted on this drug. In 1936, the son of US President Franklin D. Roosevelt contracted streptococcus pharyngitis and successfully treated with the new drug. Prontosil became fully established and allowed diseases with high mortality at the time, such as puerperal fever, to be controlled.
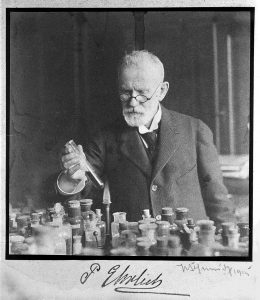
Paul Ehrlich heating a test tube in the laboratory (1915). Wellcome Collection.
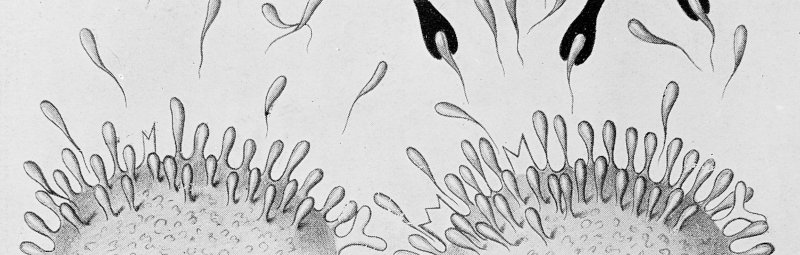
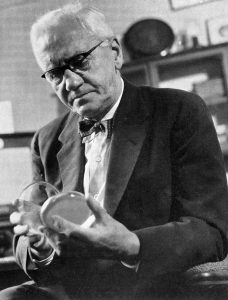
Following the Ehrlich method, a large number of sulfonamide derivatives were tested, starting with modifications in their molecular structure. The sample 693 saved Winston Churchill’s life in 1943, when he became ill with pneumonia. In the fight against microorganisms, sulfonamides gave way to antibiotics, with penicillin at the forefront. In 1928, the Scottish physician Alexander Fleming (1881-1955) was working on staphylococci at St. Mary’s hospital in London, when he found a culture dish of these microorganisms that had been left forgotten next to an open window before going on holiday. This had been contaminated with a fungus of the genus Penicillium, which eliminated the staphylococcus. Fleming soon left his research on these bacteria.
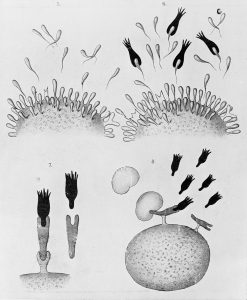
Paul Ehrlich’s theory of immunity. Wellcome Collection.
The fungus culture strain he discovered, penicillin, was successfully used in 1940 on experimental animals by the Australian pathologist Howard Walter Florey (1898-1968) with the help of the German chemist Ernst Boris Chain (1906-1979), who resumed Flemming’s work at the University of Oxford. They first developed a surface fermentation method, using glass milk bottles. Then a slow purification process was carried out. In 1941 it was tested for the first time on a man who, after recovering, ended up dying when the penicillin reserves were exhausted. Production of this began in the UK pharmaceutical industry, but the manufacturing capacity in this country was insufficient as it was involved in the Second World War. Florey went to the United States to convince pharmaceutical companies of the economic benefits and usefulness of penicillin manufacture. Pfizer laboratories did so, replacing the surface fermentation process with the more effective submerged culture fermentation process. The industrial manufacture of penicillin allowed it to be used to treat soldiers fighting in the Second World War, among many other aspects.
Mª José Báguena Cervellera
IILP-UV
How to cite this paper:
Báguena Cervellera, Mª José. ‘Magic bullets’. Sabers en acció, 2021-01-20. https://sabersenaccio.iec.cat/en/magic-bullets/.
Find out more
You can find further information with the bibliography and available resources.
Recommended reading
Puerto, Javier. El mito de la panacea: compendio de historia de la terapéutica y de la farmacia. Madrid: Doce Calles; 1997.
Santesmases, María Jesús. The circulation of penicilin in Spain. London: Palgrave Macmillan; 2018.
Studies
Grundmann, Ekkehard. Gerhard Domagk: The First Man to Triumph over Infectious Diseases. Lit Verlag: Münster; 2004.
Macfarlane, Gwyn. Alexander Fleming: The Man and the Myth. London: Chatto and Windus; 1984.
Parascandola, John. Studies in the History of Modern Pharmacology and Drug Therapy. Surrey: Ashgate; 2012.
Sources
Chain, Ernest et al. Penicillin as a Chemotherapeutic Agent. Lancet. 1940; 239: 226-228.
Domagk, Gerhard. Ein Beitrag zur Chemotherapie der bakteriellen Infektionen. Deutsche Medizinische Wocherschrift. 1935; 61 (7): 250-253.
Ehrlich, Paul; Hata, Sahachiro. Die experimentelle Chemotherapie der Spirillosen (Syphilis, Rückfallfieber, Hühnerspirillose, Frambösie). Berlin: Julius Springer; 1910.
Websites and other resources
José L. Fresquet. La Prensa diaria y la introducción en España del “606” [Updated 2012; accessed 7 July 2020]. Available here.
José L. Fresquet. Salvarsán. La bala mágica [Updated June 2020; accessed 7 July 2020]. Available here.
Paul Ehrlich-Biographical. Nobelprize.org Nobel Media AB [Updated 2014; accessed 7 July 2020]. Available here.