—Changes in healthcare organisation in Spain during the twentieth century and changes in the international arenal.—
In the first half of the twentieth century, health organisation in Spain was focused on the prevention of social dominant diseases, which were predominantly infectious: tuberculosis, syphilis, malaria, typhus, maternal and infant mortality, hunger and diseases arising from poverty and poor hygiene conditions. To prevent these, the hygiene and health of the environment (water, air, soil) and of the social environment (housing, schools, public and private spaces) were sought. Private medicine of the nineteenth century was initially practised in private clinics, where the figure of the general practitioner served all sectors of society, except the excluded, who were cared for in hospitals for the poor and charities. At the beginning of the twentieth century, municipal clinics and health campaigns, hygiene education and preventive and vaccination campaigns were the setting for medical practice in the public sphere. This was a model of social and health care based on the idea of prevention. A model articulated by municipal health administrations with scarce economic and technical resources, coordinated by national institutes of health in the central administration and other institutions of provincial and municipal character. In this institutional framework, health inspectors acted as health agents, as did nurses and especially public health visitors. There were also other institutions, such as the ‘Gotas de Leche’ (‘milk drops’) or baby-care centres and institutes, whose aim was to reduce infant mortality by providing mothers with knowledge and means for the survival of babies.

Contamination of water and foodstuffs. Illustrations published in FUN magazine in August 1866.
At the beginning of the twentieth century, the majority of the Spanish population lived in rural communities, so bringing sanitation, hygiene and assistance to rural areas became one of the political objectives. The ruling elite and the bourgeoisie were aware that disease and poverty were the main causes of underdevelopment, and vice versa, so that this spiral, which harmed social development, progress towards modernity and the well-being of the population, had to be broken. That is why, in 1883, the Spanish parliament created a social reform commission and later an institute of the same name and purpose, following a liberal reformist ideology. Later, in the early 1920s, a health commission was created to eradicate hunger and its consequences: poor organic development, cretinism, goitre and a series of mental deficiencies, especially in very poor regions such as Las Hurdes (Extremadura). In these campaigns of medical and social reformism, prominent doctors such as Gregorio Marañón and Ángel Pulido participated, with the support of the monarchy and the high spheres of the church. King Alfonso XIII and the Archbishop of Plasencia were part of the Patronage of Las Hurdes, created in 1922, to promote the carrying-out of intervention campaigns in that area. It was enough to guarantee a subsistence agricultural economy, educate the population in hygienic habits, combat hunger and iodise drinking water. Diagnostic technology and therapeutic resources were very limited, but simple medical hygiene interventions could yield considerable results.

Trip of the Spanish monarch Alfonso XIII to Las Hurdes (Cáceres, Spain). Campúa.
After the two World Wars, technical innovations, sometimes originating in wars, and new national health systems put hospital institutions at the centre of the care model. The new national health systems were founded as a space for professional specialisation and technological innovation. The most advanced medicine was no longer viable as a liberal profession exercised in the private medical practice, it required specialisation, technological infrastructures and medical equipment. This trend became more acute towards the end of the twentieth century.
Instituto Nacional de Hygiene Alfonso XIII, Madrid, 1930’s, destroyed during the Spanish Civil War. Portal Madrid+d.
From the mid-nineteenth century, cholera and yellow fever epidemics led to the imposition of restrictions by states in the form of quarantines. These measures conditioned the free movement and traffic of persons and goods. The lazaretto (leper colony) at sea and river borders, as well as the cordons sanitaires, posed difficulties for international free trade. This was the starting point for a new health diplomacy that started with international health conferences, hygiene and demography congresses, international conferences on tuberculosis, charity institutions, syphilis, and school hygiene. These meetings boosted the role of public health experts and accentuated the political dimension of health. Expert networks and representations of scientists were also expanded to agree on doses, biological standards, and serological products such as vaccines. The result was the creation of an International Office of Public Hygiene in Paris (1907) and a Health Organization at the League of Nations (1920) to alleviate the devastating effects of epidemics (influenza, typhus) and famine caused by the Great War. When an immense typhus pandemic ravaged the border territories between Poland and Russia in 1921, aware of the international dimension of this health emergency, the Heath Organization of the League of Nations promoted a conference and an international epidemic commission to curb the threat of it spreading throughout Europe. To achieve this, diplomatic tensions and armed conflicts had to be overcome. By overcoming these tensions, not without an exceptional dose of diplomacy, they was able to give rise to an ambitious international health programme funded by a philanthropic organisation, the American Rockefeller Foundation, which through its International Health Board funded programmes to train public health experts, promoted the creation of an International Epidemiology Service with headquarters in Geneva and Singapore, and a World Public Health Documentation Centre, based at the Palais des Nations in Geneva, in addition to specific programmes to advance the standardisation of biological products (vaccines, serums, nutrients, medicines), and promote programmes to prevent malaria, malnutrition, tackle opium consumption and infant mortality. The international public health experts of the League of Nations were the founding nucleus of the World Health Organization (Geneva, 1946), as the international consultative body of the United Nations on health matters.
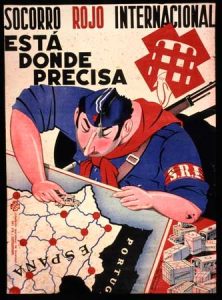
The international health conference sponsored by the World Health Organization in Alma-Ata (1978), the capital of Soviet Kazakhstan in the context of the Cold War, issued a programmatic statement that marked a new path for international health and emphasised the importance of primary care and community medicine. This opened the door to the emergence of a movement of international health cooperation with very active non-governmental organisations such as Médecins Sans Frontières, Medicus Mundi, Save the Children and countless smaller health NGOs. A century earlier, the International Red Cross had been established as a neutral organisation for the care of the wounded and sick in war conflicts. Also, in exceptional circumstances, the International Red Aid and the International Brigades had generated forms of health activism associated with a political commitment to human rights and democracy.
Josep Lluís Barona Vilar
IILP-UV
How to cite this paper:
Barona Vilar, Josep Lluís. Spaces for health action. Sabers en acció, 2021-02-08. https://sabersenaccio.iec.cat/en/spaces-for-health-action/.
Find out more
You can find further information with the bibliography and available resources.
Recommended reading
Barona Vilar, J.L. Health Policies in Interwar Europe. A transnational perspective. London: Routledge; 2019.
Barona Vilar, J.L. Salud, tecnología y saber médico. Madrid: Ed. Fundación Ramón Areces; 2004.
Berliner, H.S. A System of Scientific Medicine: Philanthropic Foundations in the Flexner Era. New York & London: Tavistock; 1985.
Brunton, D. (ed.) Health, disease and society in Europe. A source book. Manchester: Manchester University Press / Open University; 2004.
Cooter, R.; Pickstone, J. (eds.) Companion to Medicine in the Twentieth Century. London and New York: Routledge; 2003.
Livingstone, D. N., Putting science in its place: geographies of scientific knowledge. Chicago, University of Chicago Press; 2003.
Studies
Abu-Sada, C. (dir.) & Médicos sin Fronteras. Juego de Espejos. Reflexiones sobre la percepción de MSF y la acción humanitaria. Barcelona: Icaria.
Andresen, A.; Barona, J.L.; Cherry, S. (eds.) Making a New Countryside. Health Policies and Practices in European History ca 1860-1950. Frankfurt: Peter Lang; 2010.
Barona, J.L. The Rockefeller Foundation, Public Health and International Diplomacy. London: Pickering & Chatto; 2015.
Barona, J.L.; Bernabeu Mestre, J. La salud y el estado. El movimiento sanitario internacional y la administración española (1851-1945). Valencia: PUV; 2008.
Bauman, R. La medicina humanitària. Barcelona: Icaria/Médecins Sans Frontières; 2011.
Borowy, I., Coming to Terms with World Health. The League of Nations Health Organization 1921-1946, Frankfurt am Main: Peter Lange, 2009.
Bradol, J. H.; Vidal, C. (dirs.) Innovaciones médicas en la acción humanitària. El Trabajo de Médicos sin Fronteras. Barcelona: Icaria; 2011.
Hüntelmann, A. C.; Vossen, J.; Czech, H. (eds.) Gesundheit und Staat: Studien zur Geschichte der Gesundheitsämter in Deutschland, 1870 – 1950. Husum: Matthiesen Verlag; 2006.
Labisch, A., Homo Hygienicus. Gesundheit und Medizin in der Neuzeit. Frankfurt: Campus; 1992.
Marks, Shula. “What is Colonial about Colonial Medicine? And What Has Happened to Imperialism and Health?” Social History of Medicine 10 (1997): 205–19.
Page, B.B.; Valone, D.A. (eds.), Philanthropic Foundations and the Globalization of Scientific Medicine and Public Health. Lanham: University Press of America; 2007.
Petersen, K.; Stewart, J. and Sørensen, M.K. (eds.) American Foundations and the European Welfare States. Odense: University of Odense; 2013.
Saltman, R.B. et al. (ed.) Primary Care in the driver’s seat? Organizational reform in European primary care. Maidenhead: Open University Press; 2006.
Salud y cooperación para el desarrollo: Análisis constructivo y nuevas claves de futuro. Fontilles: Fontilles Foundation; 2015.
Weindling, P. (ed.), International Health Organizations and Movements, 1919-1939. Cambridge: Cambridge University Press 1995.
Sources
Buñuel, Luis. “Las Hurdes, Tierra sin Pan”. Available here.
Declaration of Alma-Ata International Conference on Primary Health Care, Alma-Ata, URSS, 6-12 September 1978.